
Introduction |
The VAAFT technique is performed for the surgical treatment of complex anal fistulas and their recurrences. Key points are the correct localization of the internal fistula opening under vision, the fistula treatment from inside, and the hermetic closure of the internal opening. This technique comprises two phases: a diagnostic one and an operative one. There is no need to know the fistula classification which obviously saves time and money. Moreover, surgical wounds in the perianal region are prevented and the risk of faecal incontinence is avoided because no sphincter damages are provoked.
Materials |
KARL STORZ Equipment is used (Fig. 1). The personal kit includes the MEINERO Fistuloscope (Fig. 2), a unipolar electrode (Fig. 3) connected to a high frequency unit, a fistula brush (Fig. 4) and a forceps (Fig. 5). Moreover, a semicircular or linear stapler and 0,5 ml of synthetic cyanoacrylate with a tiny catheter are used as well.
The fistuloscope is equipped with an optical channel, a working channel and an irrigation channel. The working length adds up to 18 cm; the use of a handle reduces
it to an effective length of 14 cm.
Fig. 1 |
Fig. 2 |
Fig. 3 |
Fig. 4 |
Fig. 5 |
The Technique |
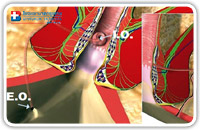 The optimal patient positioning is the lithotomic position. Spinal anaesthesia is required. The fistuloscope is connected to the KARL STORZ equipment and to the washing solution bag (5000 cc glycine and mannitol 1% solution). Fig. 6 shows an example of an anal fistula with its external (E.O.) and internal (I.O.) openings.
The optimal patient positioning is the lithotomic position. Spinal anaesthesia is required. The fistuloscope is connected to the KARL STORZ equipment and to the washing solution bag (5000 cc glycine and mannitol 1% solution). Fig. 6 shows an example of an anal fistula with its external (E.O.) and internal (I.O.) openings.
The technique comprises a diagnostic phase and an operative phase.
1. The diagnostic phase
The purpose of the diagnostic phase is the correct localization of the internal fistula opening.
The fistuloscope is inserted through the external fistula opening with the washing solution (glycine 1% and mannitol 1%) already running; providing a clear view of the fistula pathway which appears on the screen (Fig. 7). Blocking tissue can be removed using the 2 mm forceps to facilitate the insertion of the fistuloscope. The direction of the telescope is correct when the obturator appears in the lower part of the screen (Fig. 8).
Fig. 7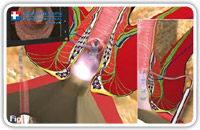 |
Fig. 8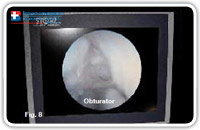 |
The surgeon follows the fistula pathway using slow left-right and up-down movements. Since the fistuloscope is rigid it helps to guide it using a transanally inserted finger. These maneuvers are favored by the complete relaxation of the surrounding tissue induced by the spinal anesthesia.
The continous flow of the glycine-mannitol solution allows for an optimal view of the fistula’s inside up to the internal opening.
The assistant can insert an anal retractor in order to localize the internal fistula opening by looking for the light of the telescope in the rectum or anal canal. Dimming the lights in the operating theatre enables an easy localization of the fistuloscope light in the rectum.
When the fistuloscope exits through the internal opening the rectal mucosa clearly appears on the screen. (Fig. 9–11).
Fig. 9 |
Fig. 10 |
Fig. 11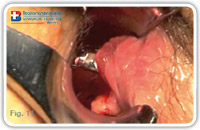 |
The Technique |
At this point, we put two or three stitches in two opposite points of the internal opening margin in order to isolate and, above all, not to loose it. We must be sure to capture sufficient tissue thickness (Fig. 12–14)
Fig. 12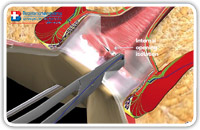 |
Fig. 13 |
Fig. 14 |
2. The operative phase
Purpose of this phase is the destruction of the fistula from the inside. As a next step, the fistula canal is cleaned / the waste material removed and its internal opening is then closed hermetically. We start destroying the fistula under vision using a unipolar electrode which can be passed through the operative channel of the fistuloscope and is connected to the electrosurgical power unit (Fig. 15–18).
Fig. 15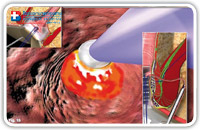 |
Fig. 16 |
Fig. 17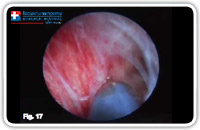 |
Fig. 18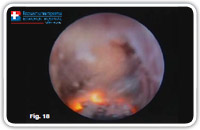 |
Starting at the internal fistula opening, all fragments of the whitish material adhering to the fistula wall and all granulation tissue are coagulated. We omplete this phase of the operation, centimeter by centimeter, from the internal opening to the external opening not forgetting any abscessual cavity.
The Technique |
The necrotic material is removed under vision using the fistula brush (Fig. 19–21). Until that time, the solated internal fistula opening remains open to allow the leakage of waste and washing material into the rectum.
Fig. 19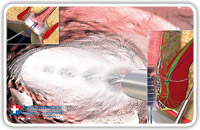 |
Fig. 20 |
Fig. 21 |
At this point we completely remove the fistuloscope. The assistant stretches the threads towards the internal rectal space or rather the anal canal using a straight forceps in order to lift the internal fistula opening at least 2 cm into the shape of a volcano. Subsequently, we insert a stapler (e.g. CCS30 Transtar Contour from ETHICON EndoSurgery) at the volcano’s base (Fig. 22–25) and complete the mechanical cutting and suturing.
Fig. 22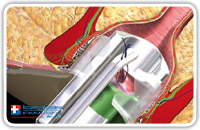 |
Fig. 23 |
Fig. 24 |
Fig. 25 |
The Technique |
The hermetic closure of the internal fistula opening can also be accomplished by using a linear stapler (Fig. 26–28). This also depends on the internal opening position.
Fig. 26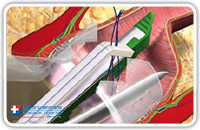 |
Fig. 27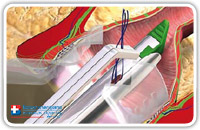 |
Fig. 28 |
Using a semicircular stapler, the suture will be horizontal. Using a linear stapler, the suture will be vertical (Fig. 29–31)
Fig. 29 |
Fig. 30 |
Fig. 31 |
When the tissue in the area of the internal opening is not sclerotic and allows to form a good “volcano”, the stapler can be used, however if the tissue around the internal opening is too rigid and sclerotic, the use of the stapler might be difficult. In this case a cutaneous mucosal flap would be preferred (Fig. 32).
Fig. 32 |
As a last step we insert 0,5 ml of synthetic cyanoacrylate right after the suture / staple line via the fistula pathway to further reinforce the suture.
So the use of the synthetic cyanoacrylate behind the suture line or behind the flap assures the perfect opening closure. It is essential to keep in mind that not the whole fistula tract is filled up with the synthetic cyanoacrylate; only a small amount is inserted directly below the suture line. That’s why the fistula pathway has to stay open to allow the passage of secretions. (Fig. 33–36).
Fig. 33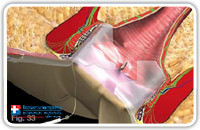 |
Fig. 34 |
Fig. 35 |
Fig. 36 |
This procedure assures a perfect excision and a hermetic closure of the internal fistula opening, excluding the risk of stool passage. Since the suture is situated tangential to the sphincter, the postoperative pain is low even if the suture falls both in the anal canal and the rectum.
Remark:
- This information should not be used as a substitute to consultation from a physician. Always talk with your doctor about diagnosis and treatment information.
- The service center is Bangkok-Phuket Colorectal Disease Institute of Bangkok Hospital Phuket.
- If you have any enquiry or want to make appointment, please feel free to contact us at [email protected]






